Neisseria meningitidis serogroup X (a New serogroup) and W135 are detected in Ethiopian bacterial meningitis patients
Background
The population living in countries of the meningitis belt of Africa stretching from Senegal in the west to Ethiopia in the east are facing frequent epidemics of meningitis. The first report on the outbreak of meningitis in Africa was documented in 1840 (1). Major epidemics of meningitis were reported earlier in African countries such as Nigeria and Ghana in 1905-1908 and in Ethiopia in 1901 and 1935 (2). Since 1935, no single decade has passed without occurrence of meningitis epidemic in Ethiopia,and the most recent epidemics occurred in 2000 and 2003 (3,4,5). In the past two decades, the dominant meningococcal serogroup causing the disease in the meningitis belt countries was mainly serogroup A (4, 6, 7), followed by serogroup C (8, 3). However, the presence of other serogroups wasreported from meningitis belt countries in later years (3).surveillance is suggested to predict receptive areas at risk of malaria outbreaks in low transmission settings. The aim of this policy brief is to foster dialogue and decisions that are practiced by the best available evidence in the malaria prevention and control endeavors.
Detection of the exposure to malaria parasites as a viable means for malaria elimination: Evidence from serological assay
Summary
Ethiopia has realized a sustained decline in malaria burden comparing to most malaria endemic countries. Nevertheless, there is a need to foster dialogue and decisions that are practiced by the best available evidence in the malaria prevention and control endeavors.
A combination of methods including microscopy, molecular assays and serology were used to examine the current burden of malaria and history of malaria transmission among 1,144 samples, 46 – 128 per village, in Babile district, Ethiopia.
The study supported that Serology can be adapted as an alternative tool to monitor malaria elimination effort of the malaria program with relatively less technical demand. Thus, district-based serological surveillance is suggested to predict receptive areas at risk of malaria outbreaks in low transmission settings. The aim of this policy brief is to foster dialogue and decisions that are practiced by the best available evidence in the malaria prevention and control endeavors.
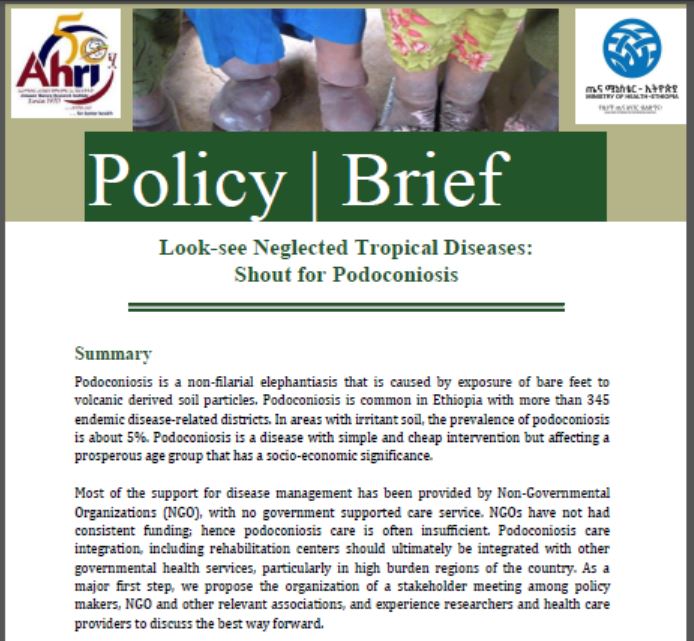
Look-see Neglected Tropical Diseases: Shout for Podoconiosis
Summary
Podoconiosis is a non-filarial elephantiasis that is caused by exposure of bare feet to volcanic derived soil particles. Podoconiosis is common in Ethiopia with more than 345 endemic disease-related districts. In areas with irritant soil, the prevalence of podoconiosis is about 5%. Podoconiosis is a disease with simple and cheap intervention but affecting a prosperous age group that has a socio-economic significance.
Most of the support for disease management has been provided by Non-Governmental Organizations (NGO), with no government supported care service. NGOs have not had consistent funding; hence podoconiosis care is often insufficient. Podoconiosis care integration, including rehabilitation centers should ultimately be integrated with other governmental health services, particularly in high burden regions of the country. As a major first step, we propose the organization of a stakeholder meeting among policy makers, NGO and other relevant associations, and experience researchers and health care providers to discuss the best way forward.
Flow cytometry for the diagnosis of acute leukemia in Ethiopia
Summary
Flow cytometric phenotypic has become one of the principal means of diagnosing acute leukemia, and is routine in many western settings to guide patient management. The Armauer Hansen Research Institute has over 30 years of experience in flow cytometry, and has conducted several research pilot studies into its use for leukemia diagnosis in the Ethiopian setting. Our findings confirm results of many previous clinical studies and have demonstrated the feasibility of this approach for many patients and the hematologists and pathologists at Black Lion hospital are enthusiastic about its application; however, the cost and technical and interpretative skill required is not trivial.
We propose a two-phase plan of implementation of flow cytometry phenotyping. The first phase will last two years and focus on intensive training and gradual roll out with comprehensive monitoring at Black Lion hospital. After review of strengths and weakness of the program, a second phase will be entertained, in which appropriate modifications will be introduced, including expansion of involved sites to peripheral oncology centers and upgrade of flow cytometers.